Many different medicines have been tested for treatment against the covid-19 virus. Through trial and error, some have been found to benefit recovery while others have had little impact. One thing is for sure, should you become severely ill, oxygen supplementation is crucial. Other than that, preventative measures are still our best combatant against the virus.
Getting vaccinated is the best thing you can do to avoid getting ill with Covid. But even some vaccinated people become very ill from the disease. Good care in hospitals is essential, and has been saving many lives.
The science of treating Covid has a long way to go, but there are some treatments that have been shown to help, and there are promising new medicines. There were also some overhyped ones which turned out to be disappointing.
Most people who get Covid won’t need any medicines, except perhaps paracetamol for pain relief, but a large number of people — the exact percentage is hard to estimate — become ill enough to go to hospital.
Guidelines on how to treat people with moderate or severe Covid are long, complicated documents (United States, South Africa) — and for good reason: this is a complicated disease. Exactly how to treat a particular person requires trained medical expertise. The information here is merely a bird’s eye view and this article does not replace the considered case-by-case decisions made by expert doctors.
Oxygen
Oxygen has been the most important “medicine” for people in hospital with Covid. Of course you take in oxygen every time you breathe, but we are talking about supplemental oxygen when you can’t get enough into your lungs and blood because of the damage Covid does to the lungs. There are two ways oxygen is administered:
- Most people are given high-flow non-invasive oxygen. A device is attached to their nose to allow them to breathe in fast-flowing oxygen. Importantly, they breathe on their own. Outcomes have been good, with most patients surviving and gradually recovering their health.
- Very sick patients are connected to ventilators which breathe for them. They have to be sedated, often for weeks, even months. Most patients at this stage do not make it.
More about this is explained by Spotlight.
How do you know when to go to hospital? One clear sign is if you are experiencing increasing breathlessness.
Also helpful, if you can get hold of one, is a pulse oximetry device. Many of these have been circulating during the pandemic from one household to the next, so find out from friends and family if they have one.
You clip the device onto your finger and it instantly measures how well your lungs are getting oxygen into your blood. The measurement is called peripheral capillary oxygen saturation or SpO2. A healthy SpO2 is 95% or above.
If you have Covid and your SpO2 is below 94% you are likely to have severe Covid and need to consider going to hospital for evaluation and perhaps getting supplemental oxygen. If it’s consistently below 90% you will definitely need to be on supplemental oxygen.
Lying in a prone position
Patients on oxygen will be encouraged to lie on their tummy (in a prone position), as shown below. Amazingly this simple intervention can make a big difference as this study found.
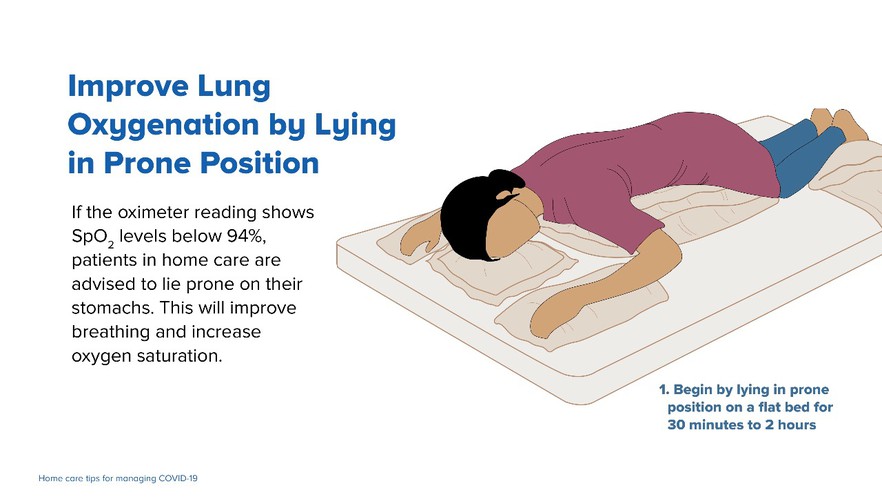
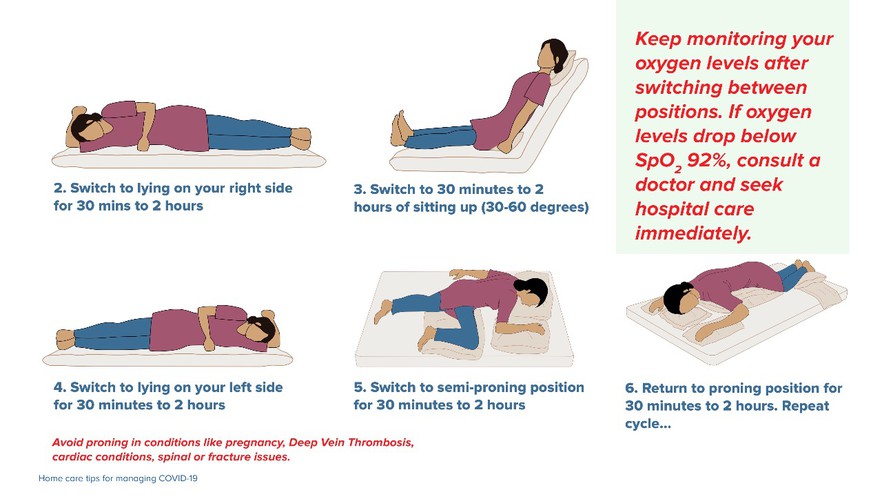
Source: Government of India
Although this seems easy, people have to move about. Health workers therefore have to move very ill patients into different positions every couple of hours. It takes organisation and planning.
Steroids
Until a few weeks ago the most effective proven medicine for treating Covid was steroids.
The South African national guidelines recommend that a steroid called dexamethasone (or its equivalent), be given to patients who are admitted to hospital and require oxygen (6mg per day for 10 days). This can be substituted with prednisone (40mg per day for 10 days) — a steroid that works very similarly to dexamethasone — if dexamethasone is not available.
Dexamethasone was shown in a large clinical trial (known as RECOVERY) to reduce the risk of death in patients needing oxygen.
Steroids remain the main type of drug used in South African hospitals to treat people with Covid. But they are unnecessary for patients who don’t also require oxygen therapy. So if you have mild Covid symptoms, there’s no need to nag your doctor for prednisone.
Incidentally, prednisone is readily available in the public health system. There are lots of generics and it’s reasonably priced (less than R160 for 1,000 5mg tablets in the private sector). This disproves the false claim circulating that research is only being done on expensive drugs to treat Covid. In fact, there have been many studies that have looked at low-priced drugs. But few have been shown to be effective.
The South African guidelines also tentatively recommend (suggest is the word used) heparin, a blood thinner, for hospitalised Covid patients. This is to reduce the risk of blood clots for which there is a high risk with Covid, and because many people hospitalised with Covid are already at high risk of blood clots. The recommendation is tentative because there is little evidence to support the use of heparin in the treatment of Covid.
Baricitinib is another medicine that has been shown to slightly reduce the risk of death of people hospitalised with Covid. But the drug, which is quite new, under patent and very expensive, is not generally available in South African health facilities.
What medicines are not used?
It may seem strange to list medicines that don’t need to be used but the desperation caused by the pandemic has led to many overzealous or premature drug recommendations.
The South African guidelines state that there isn’t enough evidence to use interferon beta, intravenous immunoglobulin, tocilizumab, azithromycin, convalescent plasma, or favipiravir outside of a clinical trial, as well as statins and some vitamin supplements.
The guidelines also state that no recommendation has been made to use the controversial antiviral drug remdesivir because of its “high cost and marginal benefit”.
Remdesivir is used in the United States, but frankly the evidence of its benefit is underwhelming. The World Health Organisation has recommended against using it because the “evidence suggested no important effect on mortality, need for mechanical ventilation, time to clinical improvement, and other patient-important outcomes”. You can’t get clearer than that.
While hydroxychloroquine and ivermectin have been hyped, the evidence is now clear that both of these drugs are ineffective against Covid. In fact, studies that showed an apparent benefit from ivermectin have been withdrawn because data had been incorrectly analysed or even forged.
A trial showed that colchicine, an anti-inflammatory used to treat gout, slightly reduced the risk of hospitalisation for people with Covid confirmed by a PCR test, but this was a subset of patients in the trial. Overall the trial showed no benefit. The US guidelines say there’s insufficient evidence to use colchicine and the South African guidelines say that the evidence is “currently undergoing review, and caution is advised until this review is complete”.
A promising drug is called fluvoxamine. It did well in a clinical trial in Brazil. In high-risk patients diagnosed early with Covid, it reduced their risk of hospitalisation. But some technical concerns have been raised and there will likely be some debate and further research before fluvoxamine is added to Covid treatment guidelines.https://www.youtube.com/embed/3SRR61o0IUM
What the near-future holds – two exciting drugs
There has been exciting news the past couple of weeks. Pfizer announced the results of a clinical trial that showed that its drug Paxlovid “reduced the risk of hospitalization or death by 89% compared to placebo” in people with Covid.
Paxlovid consists of two drugs: PF-07321332 (Pfizer’s test name, which will undoubtedly change shortly) and ritonavir. The former interferes with a Covid viral enzyme called protease, preventing the virus from reproducing, and the latter (ritonavir), which is also used to treat HIV, boosts the amount of drug your body absorbs.
The results have not yet been peer-reviewed or published in a reputable journal and no regulatory body has yet approved Paxlovid. Also, we don’t yet know enough about the drug’s safety profile and its interactions with other drugs, like HIV ones. But unless there is something wrong with the way Pfizer has conducted the trial, we should expect this medicine to be available in many countries very soon.
Also exciting is Merck’s antiviral drug molnupiravir. It reduced the risk of hospitalisation and death by nearly half. Although results from different clinical trials are not easily compared, this is much lower efficacy than was found in the Paxlovid trial, so molnupirivar is likely less effective. But an expert in the field informed us that it has fewer drug-interactions than the Pfizer one, and is easier to make.
Other than that molnupiravir has already been approved in the UK, the same cautious concerns we expressed about Paxlovid apply.
A key question is how far back in line are African countries to access these medicines? And what will their prices be? We’ll look at that in an upcoming article.
Thanks to Prof Francois Venter and Prof Marc Mendelson for reviewing the draft. GroundUp takes sole responsibility for any errors.
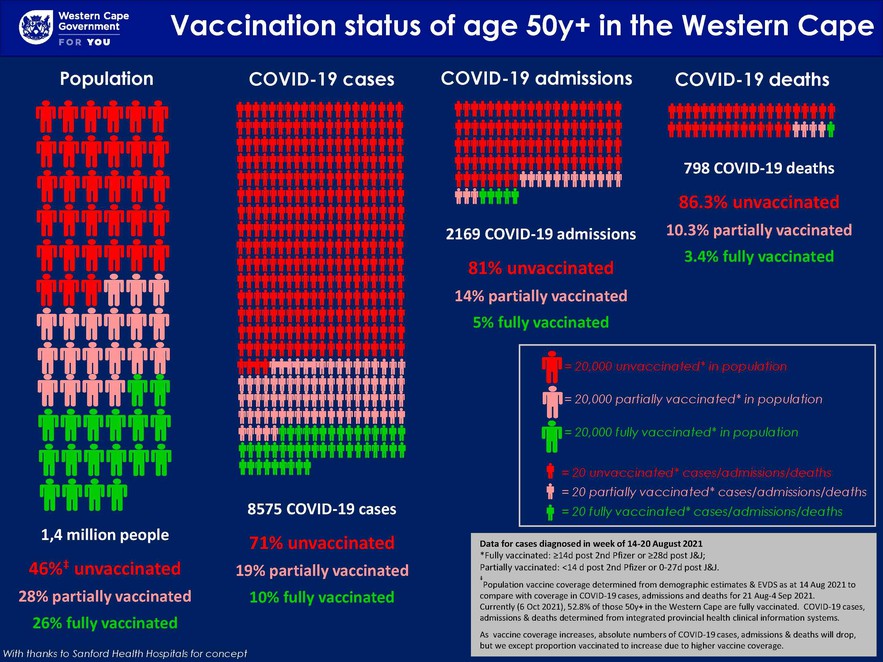
The best way to reduce the risk of needing Covid medicines is to get vaccinated as this data from the Western Cape government shows.